Page 6 - Mecklenburg_Medicine_February-2016
P. 6
Feature
Is It Possible to Improve Quality
While Decreasing Healthcare Costs?
By Anita V. Schambach, RN, MSN, CCPGM Network Director
U se of area emergency departments (ED) is down 16.7
percent in the Medicaid population, thanks to a collaboration The United States ranks 50 out of 220 countries for life
between local health professionals in Mecklenburg, Anson expectancy, but it has some of the best cancer care and survival rates.
In 2008, 1 out of every 2 people over age 18 had one of the following
and Union counties. Community Care Partners of Greater chronic conditions: cardiovascular disease, arthritis,
Mecklenburg (CCPGM) launched the initiative in 2012 to reduce non- diabetes, asthma, cancer,
urgent emergency department usage among high-risk Medicaid recipients chronic obstructive High emergency room
in the region. This work resulted in 29,000 fewer ED visits in our network pulmonary disease
alone from 2013 to 2014. A broad spectrum of local providers participate (HealthyPeople.gov). But usage is expensive,
in the collaboration, including CCPGM staff, pharmacists, county-provided over the same time period, but more important,
services, emergency medical services, Carolinas Medical Care behavioral infant mortality rates have
health providers, and the emergency department leaders and social workers continued to decline. can be a signal that
at Novant Health and Carolinas HealthCare Systems. There are many
Before we formed the collaboration and initiated more intensive determinants of health, patients might not
efforts in care coordination, emergency department utilization rates for be getting sufficient
patients were higher than the state average. High emergency room usage including genetics,
socioeconomics, individual
is expensive, but more important, can be a signal that patients might not behavior, policies and primary care and
be getting sufficient primary care and follow-up for chronic conditions. access to care and healthcare
Patients get better care at a lower cost when we coordinate treatments services that affect our follow-up for chronic
and foster collaboration between physicians and other clinical partners. health status. At CCPGM, conditions.
CCPGM now has numbers below the state average for Medicaid ED our work with 170,000
usage. And because ED visits can lead to sometimes unnecessary Medicaid recipients seeks to
hospitalizations, inpatient rates have decreased, as well. address these determinants
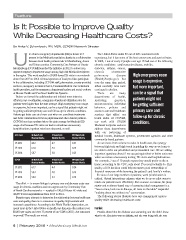
CCNC Total ED Rate/1,000 IP Rate/1,000 PPR Rate/1,000 with our partnering of
Member Months Member Months Member Months medical homes, healthcare systems, government agencies and other
community-based partners.
CY 2012 66.2 4.7 0.37
As we move from volume to value in health care, the synergy
CY 2013 61.0 4.5 0.29 between high tech and high touch is guiding the way as we learn to
CY 2014 58.7 3.8 0.23 use data to drive our prioritized and personalized care. We are asking
important questions about if we can get equivalent or better outcomes
CCPGM ED Rate/1,000 IP Rate/1,000 PPR Rate/1,000 when we reduce unnecessary testing, ED visits and hospitalizations.
Member Months Member Months Member Months For example, 7 out of 10 people report they would prefer to die at
CY 2012 home; according to the CDC, only about 25 percent actually do. This
61.7 4.4 0.34 quality-of-life decision could help us ensure good stewardship of
CY 2013 58.4 4.0 0.25 financial resources while honoring the patient’s and family’s wishes.
CY 2014 54.0 3.3 0.19 In view of our large number of patients, work prioritization is
critical. Virtual interactions enhance what we do as we pilot ways to
The effort — to ensure linkage to primary care and decrease acute care touch our patients more effectively. But on some occasions, the jump
usage for chronic conditions and non-urgent care by Community Care starter and evidence-based way of assessing ideal management is a
of North Carolina networks — resulted in 150,678 fewer ED visits and “face-to-face, look-me-in-the-eye, all facts on the table” respectful
42,477 fewer hospitalizations from 2013 to 2014. “nothing about me without me” conversation.
Despite many attempts to determine the relationship between healthcare The following stories illustrate how care management ensures
costs and quality, there is no consensus on quality improvement with quality while decreasing healthcare costs.
increased expenditures. According to the World Health Organization, we Frankie
spend more in the United States on health care than any other nation (over
$8,000 per capita and over 17 percent of our GDP in 2011). Are outcomes Frankie shared that her diabetes was worsening, and she didn’t know
improved? The results are mixed. what to do. Her sister was on dialysis, and she was being told she was
6 | February 2016 • Mecklenburg Medicine